|
Your life should be charmed and relatively stress-free. You’ve worked hard for it! But then health problems get in the way. They may not even be yours. The slow creep into a caretaker role is a real phenomenon — whether you’re caring for an aging relative or spouse. But even if you (or a loved one) hesitate to acknowledge this role, there’s no immunity from its stress.
Whether you’re a caregiver or an individual suffering from peripheral neuropathy, getting proactive is essential to less stress and a better life in Reno-Tahoe.
0 Comments
Reno, Nevada, ranks consistently as one of the best small cities in the United States thanks to its picturesque setting, rich cultural heritage, and delectable food scene. Of course, driving is one of the best ways to get around. As we age, however, it can become increasingly difficult to function behind the steering wheel, especially with peripheral neuropathy.
Nerve damage caused by the condition can lead to loss of mobility, balance issues, reduced independence, and even driver’s license suspension. But it doesn’t have to be this way. Here’s how to lead your best life in Reno-Tahoe and keep your driver’s license, even with a peripheral neuropathy diagnosis. Forbes declared Reno the best small city in the United States in 2020. And it’s not hard to see why. The “Biggest Little City” has gained international recognition for its vibrant art scene, tech innovation, and culture.
It has a distinctly cool, big-city vibe with countless micro-breweries, Brooklyn-style patios and restaurants, and much more. And it sits in the foothills of the Sierra Nevada, providing instant access to endless outdoor activities, from hiking to biking, golfing, and more. But if you’re suffering from peripheral neuropathy, this condition could be putting a serious cramp on your lifestyle in Reno. Fortunately, new therapeutic options provide a better long-term prognosis for peripheral neuropathy. Here’s what you need to know about leading your best life in Reno-Tahoe, even if peripheral nerve damage has gotten you down. If you’re a type 2 diabetic, either for many years or recently diagnosed, I want you to look at your feet:
What do you see? Hopefully they look “okay”. Sometime in the future, however, they will begin to change in appearance – it’s inevitable. The color will change; they might feel cool or cold; the skin will appear dry and flaky; at some point, redness may develop, which may be followed by a darkening of the toes. This is the first sign of gangrene. Blood spots may appear as the skin begins to break down. This is the first sign of a small, innocuous wound or ulcer. Untreated, the wounds will get bigger – a potential amputation may eventually be necessary. You may not even feel the wound. The loss of feeling and poor circulation are signs of Diabetic neuropathy. Scary, right? However, there is a way to preserve blood flow: locally applied near-infrared light therapy can release nitric oxide from red cells; nitric oxide is the body’s vasodilator, but high blood sugar destroys nitric oxide. So, when you are told to reduce A1c, there’s a very good reason! At the first signs of skin breakdown or loss of feeling, you should tell your doctor. Remember: it’s your feet – this is why I want you to LOOK AT YOUR FEET right now, and then every week from now on. Once a surgeon has to amputate, there is no turning back. Happy Thanksgiving! You’ve been diagnosed with diabetes: NOW you need to be aware of your feet and watch out for foot ulcers. Remember loss of feeling (sensory loss) is one of the signs of DPN. Foot ulcers are sores that develop on your feet, and they can develop even from seemingly trivial injuries to the feet. Diabetic foot ulcers are a common cause of amputation due to diabetes. Each year over 70,000 foot or lower leg amputations occur in diabetic patients. These folks didn’t pay attention their feet. If you lose feeling in your feet you may develop a wound that eventually becomes too difficult to heal and, to save your life, an amputation is necessary. Would light therapy, administrated early on, help lower these statistics? Probably. Why? Because it increases blood flow to the foot and its nerves and thus your sensory nerves will be able to signal something is not right in the skin of the foot. You’ll seek out health care from diabetologists and podiatrists. Remember red and near infrared light therapy increases the release of nitric oxide (NO) from hemoglobin thereby increasing blood flow to sensory nerves. The increased blood flow also brings wound-healing proteins to the wound and white blood cells that fight infections.
Dr. Thomas Burke, PhD Published researcher of 92+ papers on blood flow and peripheral neuropathy Nerves send pain signals to the brain. They also let you know if something is touching your skin. These nerves require blood flow through arteries and eventually capillaries. Nerves that are not getting good blood flow can’t function. Think of a rubber band wound tightly around a finger: soon that finger begins to hurt - the band has cut off blood flow to the entire finger, including its nerves. How do you relieve that pain? Remove the rubber band; that restores blood flow to normal. NO MORE PAIN. So, a patient with signs of DPN has to do anything they can to restore blood flow. Blood flow is partly regulated by nitric oxide (NO). If you’ve never heard of NO, we encourage you to look it up. Three American scientists were awarded the Nobel Prize for its discovery as a regulator of blood flow. NO is carried in the blood attached to hemoglobin in red blood cells. Several years ago it was found the red and near infrared light therapy could release that NO from hemoglobin (J Mol Cell Cardiol. 2009 Aug; 47(2): 256–263.). Our Clinic uses this form of FDA cleared light therapy to improve, and often reverse, the symptoms of DPN. Less or no pain, improved sensation and, with this, better balance and a lowered risk of falls are usually seen. How important is sensation? Think of the person who can’t tell the difference between the gas pedal and the break pedal. That’s a big problem for many with DPN. Improved sensation is a quality of life issue for you and your loved ones. Our next blog post will focus on wounds and amputation in patients with DPN.
Dr. Thomas Burke, PhD Published researcher of 92+ papers on blood flow and peripheral neuropathy This post is part of an ongoing series from Dr. Thomas Burke, PhD, published researcher of 92+ papers on blood flow and peripheral neuropathy.
Being diagnosed with Type 2 diabetes is a serious health issue and you should not underestimate its possible consequences. This disease is caused by high sugar levels in the blood. Untreated, this leads to heart, kidney and eye damage and it is the result of decreased blood flow to these organs. Some diabetic patients also have show signs of damage to their legs, feet and hands; this is, not surprisingly, also caused by low blood flow. The signs are loss of feeling in the feet or hands, poor balance, and often pain that interferes with sleep. These are symptoms of something called diabetic peripheral neuropathy (DPN). Poor blood flow to the feet can result in a wound that is difficult to heal and may, on occasion, lead to an amputation of toe(s), feet or lower legs. Again, do not underestimate the possible consequences of Type 2 diabetes. Next week we’ll look at some of these symptoms of DPN and their relationship to low blood flow. Peripheral Neuropathy 101
If you are experiencing aching, piercing, burning, numbness, tingling, itching or any other symptom in your feet and legs and/or hands caused by the ravaging effects of Peripheral Neuropathy and would like to be free of these life-altering symptoms once and for all, please read this in it’s entirety. The information provided here will assist you in both understanding your pain and other symptoms as well as provide you with information on a very successful method that we use in The Neighborhood Neuropathy Center to help get rid of the pain and symptoms of Neuropathy. We do this without: Side Effects Medications Injections Surgery Painful Therapy Although there is no known medical cure for Neuropathy, there are new and exciting methods to manage, control and even reverse the damage done to the nerves caused by certain factors. If you are suffering from this debilitating condition and simply taking drug after drug trying to alleviate your condition, you’re not alone. It is estimated that over 20 million Americans suffer from Peripheral Neuropathy and that doesn’t even include the number of Americans who are diagnosed with Diabetes everyday and who will eventually develop this condition. If you are one of these people, you know first hand what it’s like to be unable to do the things you like because of the constant tingling, pain, numbness and loss of feeling in your feet and legs. There is nothing more tragic than feeling you are unable to be fully engaged in the life that you have worked so hard to attain. Your zest for life and your enthusiasm for living may be greatly diminished by this pervasive and intruding pain and numbness which is affecting everything you do.  There are some surprising statistics about how common diabetic foot ulcers are, how often they can lead to amputation and the ultimate cost of having a foot ulcer that results in an amputation. 1. A foot ulcer is the initial event in more than 85% of major amputations that are performed on people with diabetes. 2. In the United States, every year about 73,000 amputations of the lower limb not related to trauma are performed on people with diabetes. 3. Of non-traumatic amputations in the United States, 60% are performed on people with diabetes. 4. Throughout the world, it’s estimated that every 30 seconds one leg is amputated due to diabetes. 5. 10% of people with diabetes have a foot ulcer. Doctors take many different paths after graduation. Just as an MD degree may lead one toward radiology, pathology or cardiac surgery, DC’s may focus on sports medicine, low back pain, or, more recently, neuropathy. Neuropathy is diagnosed when patients complain of pain, tingling, trouble sleeping, loss of sensation to heat or cold or pressure, or numbness.
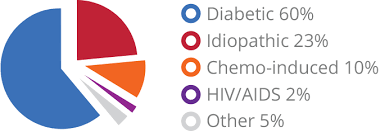
Clearly all neuropathy is not the same. To help a patient with neuropathy, one needs to know what causes his or her neuropathy. It can result from traumatic injuries, infections, metabolic disorders, and exposure to toxins. One of the most common causes of neuropathy is diabetes. And there are more than 20 million diabetics in this country. Restoring sensation and balance leads to fewer falls, which should translate into fewer fractures; restoration of sensation and balance allows patients to engage in exercise programs recommended by healthcare groups such as the American Diabetes Association. Restoring sensation also limits the catastrophic effects of unappreciated wounds that become infected or necrotic, often leading to amputations. Interventions by physicians along with standard physical therapies in such patients saves healthcare dollars and improves activities of daily living (ADL) and quality of life (QOL). About 20% of neuropathy cases are considered idiopathic, which means they are of unknown cause. Another 50% of neuropathies are due to diabetes. In fact, about 70% of people with diabetes will develop some type of neuropathy. The remaining cases of neuropathy, called acquired neuropathies, have several possible causes, including: · Trauma or pressure on nerves, often from a cast or crutch or repetitive motion such as typing on a keyboard · Nutritional problems and vitamin deficiencies, often from a lack of B vitamins · Alcoholism, often through poor dietary habits and vitamin deficiencies · Other diseases and infections, such as kidney disease, liver disease, Lyme disease & HIV/AIDS · Poison exposure, from toxins such as heavy metals, and certain medications and cancer treatment drugs Chemotherapy can and does cause neuropathy! Cancer patients who have been treated with chemotherapy are another group who might well seek out therapists to help resolve their neuropathy. How is neuropathy treated? There are a variety of treatments available for peripheral neuropathy. They range from traditional pills and creams to special diets and therapies that stimulate the nervous system. Antidepressants are a favored treatment for neuropathies. They will relieve neuropathic pain in non-depressed persons. Another class of medicines commonly prescribed for neuropathy is that of anticonvulsants such as Lyrica and gabapentin. These medicines block calcium channels on neurons to limit pain. Opioid narcotic treatments for neuropathy are used as well to treat the condition, but are less favored because of the risk of dependency. Alternative therapies for peripheral neuropathy include cannabinoids (an class of chemicals found in marijuana), Botulinum Toxin Type A (better known as Botox), NMDA antagonists (such as ketamine), dietary supplements (such as alpha lipoic and benfotiamine), chiropractic massages, yoga, meditation, cognitive therapy, and acupuncture. As you probably know, diabetes has a significant effect on blood flow. Vessels get smaller in diameter or close off completely. The skin becomes cooler than normal, it loses its pink color, and sophisticated devices like vascular ultrasound or scanning laser Doppler can demonstrate the reduction in blood flow. Some scientists and healthcare professionals have begun to focus on how to improve blood flow to the limbs of patients with neuropathy; an added benefit of that approach is improved blood flow to nerves themselves within those limbs. Why is that important? Because any of the pharmaceutical or nutritional interventions mentioned above will be delivered more effectively to the limbs and their nerves, if one increases blood flow. Drug-free approaches:Red and infrared diodes (LEDs) emit wavelengths that have been shown to increase blood flow at the site of treatment. This means that a DC, a therapist, a physician, nurse or the patient can treat the symptoms of neuropathy, in the office or the home and, by increasing blood flow, reverse or eliminate the pain, tingling, sensory loss as well as the gait and balance problems that are classic signs of neuropathy. Acute treatment with LEDs for 30 min. or less causes an immediate, sustained (for a few hours) increase in blood flow by dilating existing blood vessels. Subsequent treatments appear to cause angiogenesis (the growth of new blood vessels) so that eventually blood flow to all areas of a treated limb (or site) return toward normal rates. |




 RSS Feed
RSS Feed
